Abstract
Introduction
Chronic thromboembolic pulmonary hypertension (CTEPH) is classed as group 4 in the present classification of pulmonary hypertension. The pathophysiology of CTEPH is complex, mainly is a consequence of prior acute pulmonary embolism with failure of thrombi to resolve and the recent recognition of added small vessel changes which impacts long-term outcomes even after surgical management. The role of thrombophilia testing in this condition has been debated. Hence, we here analyzed the utility of thrombophilia testing in CTEPH from a center in a developing country.
Methods
This is a single institution (Narayana Health City, Bangalore); retrospective study including patients ≥ 18 years of age who underwent thrombophilia workup in a diagnosis of CTEPH from January 2019 till July 2021. Tests done to evaluate thrombophilia included factor V Leiden; prothrombin F20210A mutation; MTHFR gene mutation; Protein C, S, and antithrombin deficiency; lupus anticoagulant, anti-beta2 glycoprotein I (IgM and IgG) and anticardiolipin antibody (IgM and IgG); hyperhomocysteinemia and anti-nuclear antibody testing (ANA-IF). The study was approved by the ethics committee of the institute and was carried out in accordance with the principles of the declaration of Helsinki.
Results and discussion
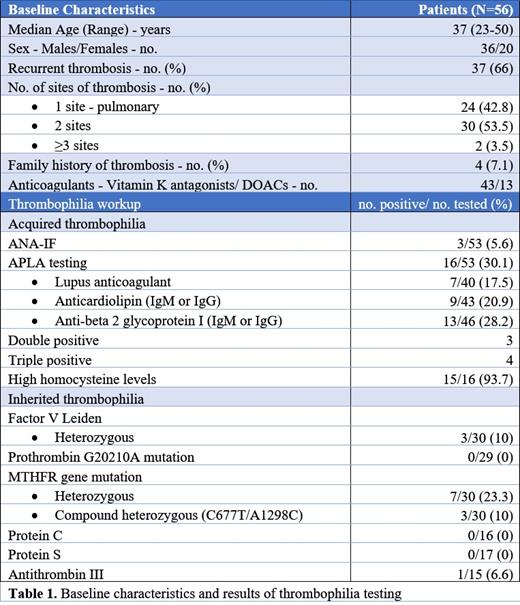
The study included 56 patients with a median age of 37 years (range 23-50), and 36 (64%) were males. Patients with recurrent venous thrombosis included 37 (66%), with the majority having thrombosis at 2 sites (53%; 22 patients with associated deep vein thrombosis). A family history of thrombosis was present in 4 patients. The majority of patients received vitamin K antagonists (76%), with the rest receiving direct oral anticoagulants (DOAC).
Among the tests sent for acquired thrombophilia, ANA-IF and antiphospholipid antibody (APLA) were most frequently evaluated (94%). ANA-IF and APLA tests were positive in 5.6% and 30.1%, respectively. Among the APLA tests, Anti-beta2 glycoprotein I (IgM or IgG) was the most commonly detected antibody (13/46), followed by anticardiolipin antibody (IgG or IgM) (9/43) and lupus anticoagulant (7/40). Double and triple positive APLA were present in 3 and 4 patients, respectively. Homocysteine levels were high in 93.7% though only 16 patients were tested in this cohort.
Among the tests for inherited thrombophilia, genetic tests (factor V Leiden, prothrombin F20210A mutation, and MTHFR gene mutation) were tested in only ~50%. Twenty-three percent were positive for heterozygous MTHFR followed by MTHFR compound heterozygous (10%) and heterozygous factor V Leiden heterozygous (10%). Antithrombin III, protein C, and S were tested in ~30% of patients. Antithrombin III was low in only 1 patient, with protein C and S assays being normal in all the patients.
The cost analysis was calculated, showed a median of $364 (₹ 27,055) was spent per person on thrombophilia workup. The median cost incurred per patient for inherited thrombophilia workup was $232 (₹ 17,300) and for acquired thrombophilia was $132 (₹ 9814), respectively.
Conclusion
This single-institution study on thrombophilia workup in CTEPH patients reveals that APLA was the most commonly performed test with high positivity rates of 30.1%. Among the inherited thrombophilia, the positivity rate of MTHFR mutation was highest (33.3%), with other tests having a low positivity rate (0-10%). Hence, we would recommend APLA testing in all patients with CTEPH considering its high positivity and clinical utility. Testing for other thrombophilias should be pursued judiciously especially in economically restrictive settings.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal